Measuring the Black Death
Reports suggest that between 40 and 60 percent of the population died during the bubonic plague that swept through Europe in the mid-1300s. What accounts for this wide range of estimates?
Saloni Dattani kicks off our pandemic mini-issue with an essay about the Black Death, and why it’s so difficult to answer a seemingly simple question: “Just how many people died from it?”
We’ll publish a new essay about pandemics, and how biotechnology can help prevent them, every day for the next three days. Read the Editors’ Note on our website for more details.
In 1346, more than five hundred years before germ theory, the Black Death spread relentlessly across Europe. Within seven years, it’s estimated to have killed around half of Europe's population.
Medieval Europeans had little idea of how to protect themselves. They didn’t know what caused the plague, how it spread, or how to prevent it, nor did they have the antibiotics that treat bubonic plague today. They also lacked institutions to count the dead; censuses, population registries, and cause-of-death records didn’t become common practice until centuries later.
Our estimates of the Black Death’s toll come from decades of research using a wide range of other historical sources, such as tax and rent registries, parish records, guild records, and court documents. Despite this, large uncertainties remain in the estimates. The case of the Black Death underscores the vital importance of statistical record-keeping, practices that we take for granted today.
Even now, many poorer countries lack such records. Without them, we struggle to learn from the past, make further progress against diseases, and track new outbreaks.
Plague Spreaders
The bacteria Yersinia pestis, responsible for bubonic plague, is ingested and carried by fleas. Y. pestis multiplies in the flea’s midgut and produces a biofilm, choking the flea until it feeds again, at which time it regurgitates the bacteria into its next host. The fleas prefer feeding on rats, living in their coats, and releasing bacteria into their bloodstream. The Y. pestis bacteria produce toxins that break down rats’ blood vessels, killing them in days. Sick and dying rats hide away to avoid being eaten alive by their kin.
Within weeks, infected rat colonies die out. As fleas lose their preferred food source, they turn to nearby humans, often biting during the night. The regurgitated Y. pestis in our skin drains into the lymph nodes, which swell and form the eponymous necrotic “buboes” in the groin, thighs, armpits, or neck.
Bacteria build up in these buboes, destroying their walls and seeping out into our bloodstream, where their toxins break down our blood vessels, much like what happens in rats. If left untreated, the bacterial toxins result in fevers, chills, vomiting, and excruciating headaches as our damaged blood vessels fail to circulate blood properly. This soon kills us.
Other fleas stow away on clothing, furniture, or even luggage, hoping to be whisked away to more plentiful lands. In the 14th century, the plague spread in just this way across Europe. It traveled most efficiently by ship, with new epidemics springing up along rivers and coasts at ports. It also journeyed overland into new communities, swiftly crippling and depleting the populace.
Only a few regions in Europe—medieval Greenland, Iceland, and Finland, where communities were small, disparate, and largely isolated from the rest of Europe by trade and migration—are believed to have escaped it.1 Centuries later, researchers poured over historical records to understand its impact. They dubbed this devastating plague “the Black Death.”
The enormous toll of the Black Death led to significant cultural and economic changes, causing a sudden loss of skilled labor and knowledge, and disrupting agriculture, crafts, and trades. “Crops went unharvested, and building projects stopped,” write the economic historians Remi Jedwab, Noel Johnson, and Mark Koyama. The decreased supply of labor boosted wages for the survivors. Many of them migrated to towns and cities, taking both the jobs and empty houses of those who had died.
The inability of religious authorities to prevent or cure the plague led to questioning of and a decline in the Church’s influence. Plague was seen as either a punishment from God or a result of insidious conspiracies: Jews were accused of poisoning wells, leading to pogroms and expulsions.
All these changes contributed to the transformation of European society before the Renaissance and the rise of early modern Europe.
Aligning History
Our knowledge of the Black Death has evolved in the past few decades as research on the topic has grown. In the 1980s, even fundamental facts like whether the Black Death was caused by Yersinia pestis came under question.
Back in 1894, Alexandre Yersin had identified the causative bacteria from post-mortem samples of buboes in patients in Hong Kong, where he was posted to help in scientific efforts against the disease. He also noted the presence of the bacteria in rats and rat fleas. Later historians, looking at the clinical symptoms and epidemiology of modern plague, made the connection between it and the Black Death, identifying both as the same disease.
But from the 1980s, some researchers argued that there were irreconcilable differences between the Black Death and modern plague. They claimed that the Black Death had spread too rapidly and killed too invariably for it to be bubonic plague, which was less fatal in the 19th century. Moreover, while Yersin had described seeing dead rats on Hong Kong’s streets, historical records from the 14th century did not contain descriptions of widespread rat deaths. This led some to believe that the Black Death was caused by a different pathogen, perhaps anthrax or a virus like influenza or even Ebola.
Others countered that the plague could have rapidly spread across the continent by means of the trading ships available at the time. Plus, rat populations declined with urbanization and hygiene, while nutrition and living standards improved, so we should expect lower mortality rates in modern times. And since rats tend to hide away before they die, perhaps their deaths hadn’t been noted by those keeping records in medieval times.
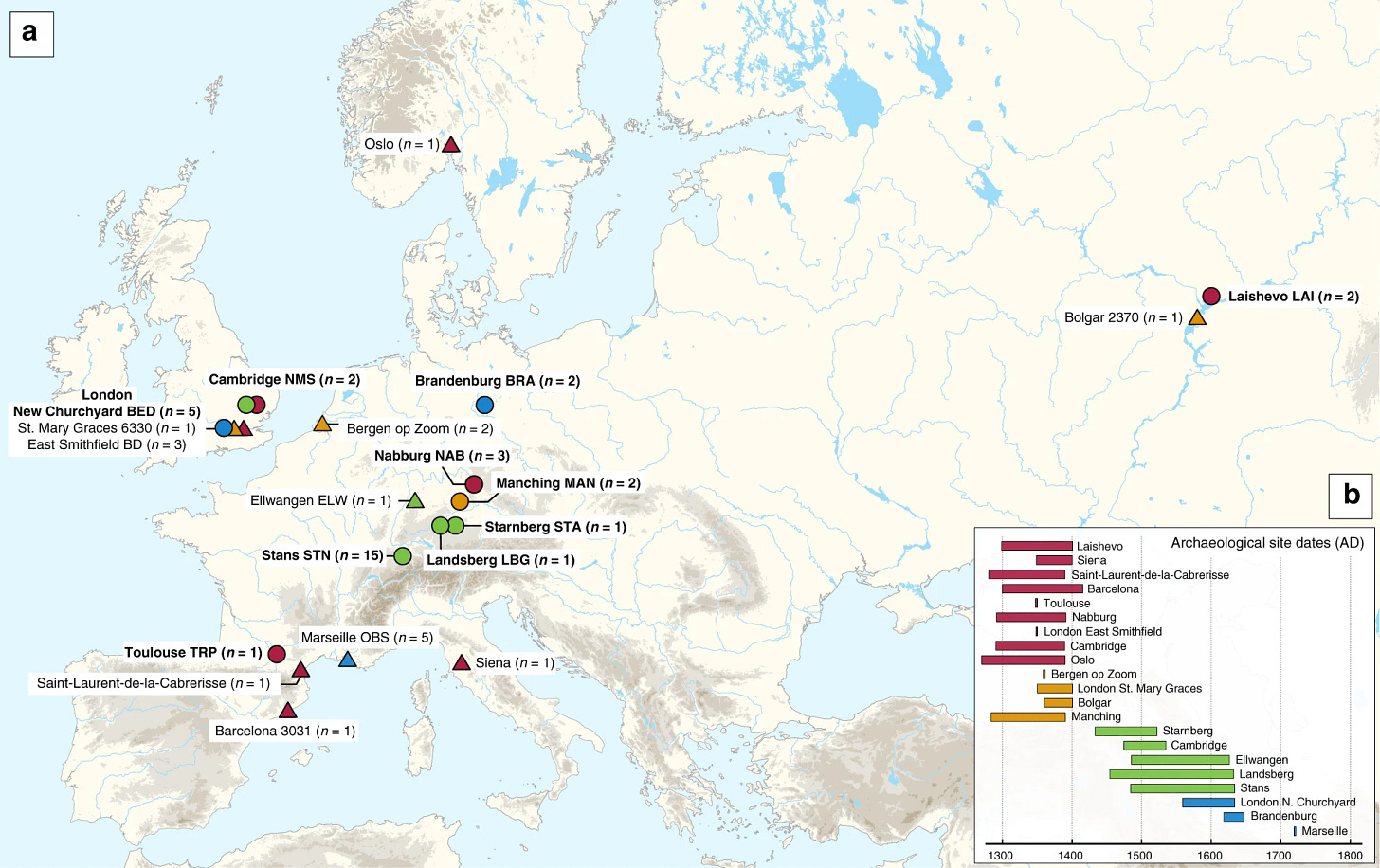
By the 2010s, this debate had been resolved. Paleogeneticists identified nearly identical strains of Y. pestis DNA in the dental pulp of skeletons in various medieval burial sites across Europe, which corresponded to recorded outbreaks, including in cemeteries used exclusively for Black Death victims. Subsequent research also showed that Y. pestis was responsible for an earlier pandemic that occurred between 541 and 750, which began with the “Justinianic Plague” (541–549 CE).
Counting Deaths
Unlike its pathogenic cause, the death toll of the Black Death is much harder to resolve.
Direct records of mortality are sparse and mostly relate to deaths among the nobility. Researchers have compiled information from tax and rent registers, parish records, court documents, guild records, and archaeological remains from many localities across Europe. However, even those who have carefully combed over this data have not reached a consensus about the overall death toll.
For example, in 2005, statistician George Christakos and his colleagues compiled data from over a hundred European cities. Using their data, the economists Jedwab, Johnson, and Koyama estimated in 2019 that 38.75 percent of Western Europe’s population had died on average. In contrast, the historians John Aberth (2021) and Ole Benedictow (2021) have estimated that 51–58 percent or upwards of 60 percent of Europe’s population died, respectively.

Most data used to estimate the Black Death’s toll comes from medieval regions in present-day Italy, England, Spain, France, and Germany—which were more urbanized than the rest of Europe. Data is thin in other countries, leaving us to extrapolate from the few localities where it is available.
Take parish records from medieval England as an example. In the 14th century, English dioceses in several areas such as York, Winchester, Coventry, and Lincoln recorded data on when parish priests were replaced. Comparing these replacements over time can be used as a rough guide for understanding the impact of the Black Death, and suggests a mortality rate between 40 and 73 percent.2
Yet there are various issues with using pastoral replacements as a proxy for mortality. Some priests may have resigned or fled rather than died, and some replacements may not have been recorded. Often priests and their successor would have both died in an outbreak before being recorded. Additionally, it was challenging to update records because many new, smaller churches and other religious institutions were being built, making it difficult for dioceses to keep track of all the changes accurately.3
Moreover, parish priests were probably unrepresentative of the medieval population as a whole. They tended to be well-fed but also older and more vulnerable to disease. They also tended to live in houses with grain stores that would be attractive to rats. Due to their duties, they were likely to have visited many families in their local area, exposing themselves to a greater risk of infection. Given these factors, they may not be representative of the mortality rate across England.
For an alternative picture, we could instead examine tax registries.
States in medieval Europe collected revenue in many different ways and for different reasons, such as poll taxes, death duties, fines, and rents. But generally speaking, they tended to exclude certain demographics: the very impoverished, young children, the nobility, the clergy, and of course, those who evaded taxes.
Moreover, taxes were payable by the heads of households, mostly men, and didn’t necessarily include data on household size. Therefore, to calculate the population size, the number of households in tax records is usually multiplied by the average household size.
This reveals two important weaknesses in how we count mortality from the Black Death.
First, we lack good historical data on the Black Death’s impact on women and children. However, we do know that modern plague has been more deadly for both due to social and biological reasons: women and children spent more time at home and women tended to care for the ill, resulting in higher exposure to rats, and pregnant women infected with bubonic plague have very high rates of abortion and/or death during pregnancy.
Second, we lack certainty regarding average household size and makeup. The Black Death led to labor shocks, migration, and social mobility, wherein laborers inherited resources and moved into housing that had been left empty. This likely affected the size and makeup of households in the following years, which would then be used as the comparison for estimating pre-plague populations.
In some cases, censuses were conducted to gather this data. An example was in the Tuscan commune San Gimignano, a self-governing area that included a town and its surrounding rural areas. In 1350, the local government sought to make good on its salt monopoly and organized a tax list similar to a census to estimate the area’s population size, so it could implement a “salt tax” on all citizens except children under seven years old.4
Comparing the 1350 tax list to the town’s previous tax list, compiled in 1332, suggests that 52 to 60 percent of the population died during the Black Death.5 (Note that 18 years elapsed between the two tax lists, which means we’re making a strong assumption that the population was roughly stable up to the Black Death.)
It might seem reasonable to assume everyone would want to be counted because salt was important for taste and food preservation. But the salt tax was costly, and households might avoid paying it for servants and maids, or claim that older children were under seven years old. And there were urban workers who commuted to Florence for day work and could bypass the tax or the need for local salt provision. This goes to show that even with detailed medieval data, we’re required to make strong assumptions in order to make estimates of the death toll.
Finally, the plague itself disrupted historical record-keeping, taxation, and burials, and caused demographic shifts, which affected records from the time. Given such limitations, how can we accurately estimate the Black Death’s toll?
One approach is to make educated guesses about some of the factors we’re unsure of, such as the average number of children, rates of tax evasion, child mortality, pregnancy mortality, and disparities between regions. This allows us to develop plausible ranges of mortality for different data sources and is what historians and demographers have done so far.
Another approach is to combine many different data sources and their uncertainties together in a single statistical model, but this has been less common.
In either case, we still face a large underlying problem. We lack sufficient data to fully understand many past pandemics. The COVID-19 pandemic, whose estimated death toll varies between 19 million and 35 million, is just the most recent example. Most of the uncertainty comes from low- and middle-income countries, which tend to have patchier data.
Or consider influenza. Since 1580, researchers believe that we’ve faced between 10 and 28 separate flu pandemics, but without further historical research and genomic sampling, it’s hard to be confident. Global mortality estimates have only been made for a handful of these flu pandemics. This includes the 1918 “Spanish flu” pandemic, whose estimated death toll ranges between 50 and 100 million deaths worldwide.
The same holds for cholera, which has caused seven pandemics in the last 200 years. Around 23 million people died from the disease in India alone between 1865 and 1947, but there are no global mortality estimates. For the third plague pandemic (1894–1940), only rough estimates have been made for India and China.
We lack knowledge of the cause of plenty of additional pandemics, such as “sweating sickness,” which led to multiple deadly outbreaks in Europe in the 15th and 16th centuries.
The Black Death isn’t an isolated case, though it happens to be one of the most well-studied. Our poor understanding is the result of a historical dearth of statistical institutions collecting data on deaths and their causes.
We don’t have sufficient data on most areas of 14th-century Europe. We lack data on the number of deaths broken down by cause from most medieval states. In fact, we generally lack data on the number of deaths in total from any cause. Even data on the total population size of Europe in history must be extrapolated from a few regions and periods, based on strong assumptions.
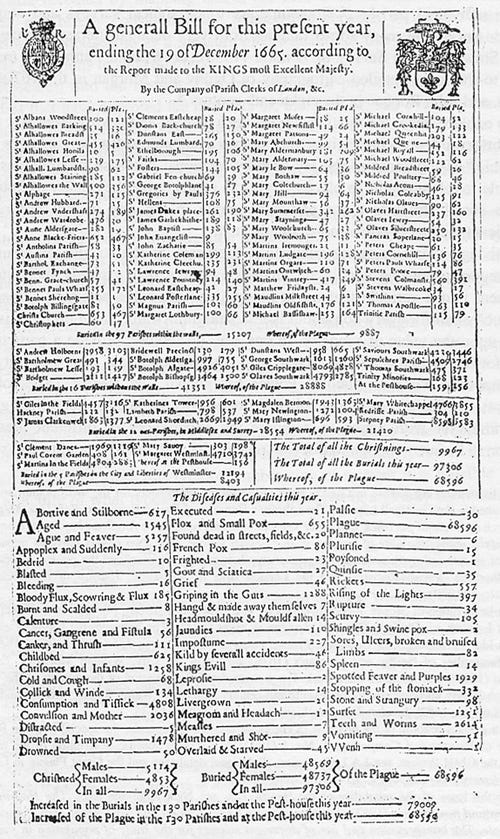
While some states collected this data in the past, it tended to be infrequent or came from select regions. London, for example, only began collecting data on the number of deaths by cause in the 16th century, to track epidemics such as plague and smallpox. England as a whole followed much later, in the 1830s.
Censuses, population registers, and cause-of-death records have been adopted by countries relatively recently. Often, these records were started in response to epidemic outbreaks, and their introduction quickly transformed our understanding of disease. One of the most famous examples is the cholera map by Dr. John Snow, who tracked cases in London during the second cholera pandemic. His work helped identify the connection between cases and traced one outbreak to a single contaminated water pump.

Many modern examples reveal a similar struggle to track deaths.
Since cause-of-death registries have been limited or dysfunctional in many countries in Africa and South Asia, some researchers have conducted national “verbal autopsies” to fill the gap. In these studies, millions of families were interviewed about recently deceased relatives and their diseases and symptoms before death. Doctors then used their answers to estimate their cause of death.
The results suggest that we had greatly underestimated the death toll of diseases such as tuberculosis and venomous snakebites. Revised international estimates suggest that they kill over 1 million and 100,000 people, respectively, each year.
But the lack of medical testing and precise hospital records means that we must extrapolate deaths and their causes from these surveys conducted in only a few countries, and often infrequently. It is hard to imagine that millions of people could die without being recorded, but that is precisely the case throughout history.
Without proper record-keeping, we can easily underestimate the frequency and severity of epidemics. Data is crucial to track their impact and identify where resources are needed—and it needs to be collected regularly and thoroughly. By fostering statistical institutions, we can make every death, or more importantly, every life, count.
Saloni Dattani is a co-founder of Works in Progress magazine and a researcher on global health at Our World in Data.
Cite: Dattani, Saloni. “Measuring the Black Death.” Asimov Press. DOI: https://doi.org/10.62211/93tr-12wn
Disclosure: Saloni is an advisor to Asimov Press.
The Complete History of the Black Death, Benedictow (2021). pp 616–619.
ibid. pp 818.
ibid. pp 792–802.
ibid. pp 711–714.
Aberth estimates a mortality rate of 52 percent in San Gimignano, while Benedictow estimates 60 percent.



Wonderful piece. Just a small suggested correction to this line:
“The scarcity of labor increased demand and wages for the survivors.”
Demand didn’t increase. The supply of workers decreased, which decreased the quantity demanded. But since the demand curve for labor is slightly downward sloping, the movement of the supply curve result in higher wages.
A really well written article. I think that the Good Doctor himself would have been proud to have it associated with his name. (I read “World Of Carbon” in 1958 while in high school, and am now an 81 year old retired chemist. The Good Doctor was a GOOD writer!)